Lockdown has tested our nation. From tussles over toilet roll to panic pasta purchases, we were unprepared for the country’s response when access to everyday goods was limited. However, it is not just our supermarket shelves that have been left with uncomfortable glaring gaps. The COVID-19 pandemic unveiled a myriad of inequalities including food insecurity and the disproportionate death and morbidity amongst the Black, Asian and Ethnic minority (BAME) and elderly population. In addition, the restructuring of health systems during this unprecedented time has resulted in many services suspended, postponed or altered to virtual consultations. Emerging data is highlighting the challenges in providing universal healthcare coverage during these changes as evidenced by the reduction in access to mental health services and concerning drop in cancer screening rates. This is creating what some have described as a ‘parallel epidemic’, where the indirect cost of COVID-19 may still take several years to fully grasp.
Healthcare access in prison
 As lockdown incrementally eases there will remain a group whose reality will not change. I am of course speaking of the prison population. Though the UK government states that prisoners get the same healthcare and treatment as anyone outside of prison, the very nature of incarceration means that the services provided by the National Health Service (NHS) are not easily translated within secure settings. Health seeking behaviours such as calling a GP, self-referring to an Emergency Department and accessing Internet or telephone triage services such as 111 are clearly limited when an individual is deprived of liberty. To claim that this same healthcare is available to the UK prison population would be at best an ignorant oversight and at worst a lie.
As lockdown incrementally eases there will remain a group whose reality will not change. I am of course speaking of the prison population. Though the UK government states that prisoners get the same healthcare and treatment as anyone outside of prison, the very nature of incarceration means that the services provided by the National Health Service (NHS) are not easily translated within secure settings. Health seeking behaviours such as calling a GP, self-referring to an Emergency Department and accessing Internet or telephone triage services such as 111 are clearly limited when an individual is deprived of liberty. To claim that this same healthcare is available to the UK prison population would be at best an ignorant oversight and at worst a lie.
Maintaining confidentiality
Another overlooked aspect of prison healthcare is the issue of maintaining confidentiality within these settings. The importance of confidentiality has been recognised through medical history from the ancient Hippocratic oath to the more modern General Medical Council advice on what constitutes good medical practice. Though disclosure of medical information usually requires consent from the patient, this is not an absolute. Disclosure without consent may be required, for example, when it is essential to protect the patient, or someone else from risk of death or serious harm.
 However, we should reflect on how readily medical information of patients in prison might be disclosed for unmerited reasons. The presence of a prison officer during a medical consultation not only undermines the principle of confidentiality but also directly affects patient care as the individual may be less willing to divulge important clinical information such as substance misuse or sexual history. This is not to say that security measures must be waived but there must be respect for confidentiality wherever feasible. Furthermore, we must recognise that detained individuals are vulnerable to paternalistic tendencies by those involved in their care. Healthcare professionals may make and act on assumptions regarding their patient’s mental capacity, leading to situations such as the attending officer being addressed rather than the patient.
However, we should reflect on how readily medical information of patients in prison might be disclosed for unmerited reasons. The presence of a prison officer during a medical consultation not only undermines the principle of confidentiality but also directly affects patient care as the individual may be less willing to divulge important clinical information such as substance misuse or sexual history. This is not to say that security measures must be waived but there must be respect for confidentiality wherever feasible. Furthermore, we must recognise that detained individuals are vulnerable to paternalistic tendencies by those involved in their care. Healthcare professionals may make and act on assumptions regarding their patient’s mental capacity, leading to situations such as the attending officer being addressed rather than the patient.
Step towards equal healthcare access
Despite these criticisms, it is important to acknowledge that we have made progress in providing universal healthcare to those detained in prisons since the official handover of responsibility of commissioning prison health was transferred from the Home Office to the NHS in 2006. This move, though belated at almost 60 years after the founding of the NHS, was a step toward recognising at least that those in prison deserved the same standard of healthcare as the general population. Steps such as this are important given that the UK has amongst the highest incarceration rates in Western Europe.
Equity rather than equality
 Yet, if there is anything that this pandemic has taught us it is that a one-size fits all approach can be dangerous practice and simply providing the same healthcare is not enough. Complex socioeconomic disparities mean that certain groups experience increased disease burden. With regards to people in prison this corresponds to a 50% increase in standardised mortality rates compared to the wider public. The average age of death for those in prison is 56 years compared to the wider UK expectancy of 81 years. Of course, the mean age in prison is much younger than the general population so we must interpret this accordingly. Nevertheless, even when we consider those formerly detained and now seemingly accessing the same services as the general population the standardised mortality rates rise even higher still!
Yet, if there is anything that this pandemic has taught us it is that a one-size fits all approach can be dangerous practice and simply providing the same healthcare is not enough. Complex socioeconomic disparities mean that certain groups experience increased disease burden. With regards to people in prison this corresponds to a 50% increase in standardised mortality rates compared to the wider public. The average age of death for those in prison is 56 years compared to the wider UK expectancy of 81 years. Of course, the mean age in prison is much younger than the general population so we must interpret this accordingly. Nevertheless, even when we consider those formerly detained and now seemingly accessing the same services as the general population the standardised mortality rates rise even higher still!
We also know that the prevalence of serious mental health problems, substance misuse and some infectious diseases are more common amongst those in our criminal justice system. Because of these differences, the goal ought not to be having the same healthcare but rather striving for the same health outcomes.
First do no harm
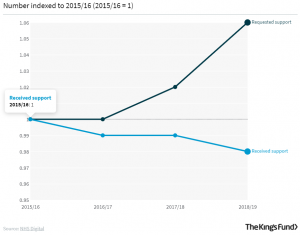 A second parallel that we must learn from this pandemic when addressing prison health is the necessity of prioritising safe living and working environments for vulnerable individuals. Sadly, many of the victims of this pandemic have been residents in care homes, exposing what has been a long time issue of underfunding social care – with an ever-widening gap between those requesting access to social care and those receiving it.
A second parallel that we must learn from this pandemic when addressing prison health is the necessity of prioritising safe living and working environments for vulnerable individuals. Sadly, many of the victims of this pandemic have been residents in care homes, exposing what has been a long time issue of underfunding social care – with an ever-widening gap between those requesting access to social care and those receiving it.
Health and social care institutions are responsible for creating environments that do not cause harm or exacerbate long term physical and mental health conditions. However, in prison settings this is falling short – and at some point we must question whether our prison system is at odds with the commitments of health and social care. All too often, people leave prison with aggravated physical and mental health.
Lessons learned?
 This is a cost we simply cannot afford. As we slowly start the journey back to life pre-lockdown we must make use of these painful lessons learned to better the health of those who will remain in prison. The World Health Organisation defines universal health coverage as ensuring that all people have access to needed health services. Health commissioning services must commit to delivering tailored approaches that address the specific needs of the prison population and improve the safety within prisons so that no one in our society is left behind. As we continue the progressive movement towards holistic and integrated health systems, we must critically reflect on how well we are also taking into consideration the needs of those in the criminal and justice system.
This is a cost we simply cannot afford. As we slowly start the journey back to life pre-lockdown we must make use of these painful lessons learned to better the health of those who will remain in prison. The World Health Organisation defines universal health coverage as ensuring that all people have access to needed health services. Health commissioning services must commit to delivering tailored approaches that address the specific needs of the prison population and improve the safety within prisons so that no one in our society is left behind. As we continue the progressive movement towards holistic and integrated health systems, we must critically reflect on how well we are also taking into consideration the needs of those in the criminal and justice system.
If you work in health and would like to explore and take action on issues related to prisons, policing and health, please e-mail [email protected]
To receive updates about Medact’s work on Securitisation and Health, sign up to our mailing list
Further reading
Aiyan Maharasingam, ‘Out of sight – facing coronavirus incarcerated’ (2020)
Reem Abu-Hayyeh, ‘Mental health and deaths after police contact – why Seni’s Law is welcome but more is needed’ (2018)
Sarah Lasoye, ‘On Tasers, policing and imagining new responses to violence’ (2019)
Frank Arnold, ‘First Do No Harm: Clinical roles in preventing and reducing damage to vulnerable immigration detainees’ (2017)